Texas Nurses Flex their Voice about HIT
![]() Print this Article | Send to Colleague
Print this Article | Send to Colleague
Texas Nurses Flex their Voice about HIT
Cynthia Plonien DNP, RN, CENP
Nursing leadership plays a critical role in managing systems of information technology (IT). While advantages of the electronic health record (EHR) to providers and organizations are frequently cited by evidence, evaluating concerns are less frequent. As EMRs are implemented and processes and procedures become standard within organizations, our attention has turned to usability, satisfaction, and unintentional outcomes. Questions asked by many nurse leaders include: How are nurses affected by EHRs? Does IT work flow create or impair efficiency? Is work satisfaction increased or decreased? Is critical thought enhanced or diminished? Is patient safety improved or compromised?
In a national survey, 79% of physicians reported that their practice ran more efficiently with electronic health records. Efficiencies were specifically noted in relation to integrated scheduling, e-prescribing, automated formulary checks with health plans, accuracy in coding, turn-around time on lab and diagnostic imaging, and access to patient data from literally any location.1
From a financial perspective, Juniper Research reported an expected savings of 78 billion between 2014 and 2019 as IT saturates health care markets worldwide2 . Federal mandates have made it clear that EHRs are necessary for maintaining reimbursement for patients insured through Medicare and Medicaid, however, identifying a true return on investment (ROI) is complicated. The direct costs associated with implementation include purchase of an EHR, licensing fees and implementation expense. Direct costs can be calculated. Adapting EHRs to meet needs of specific organizations incur indirect costs correlating to productivity that are often difficult to assess. At present, overall increases in revenue that are reported by organizations appear to be related to improvements in coding3.
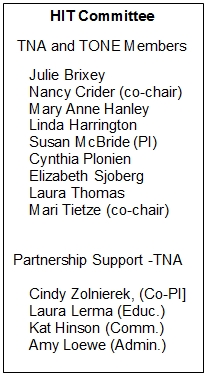
Additional indirect costs are attributed to usability and satisfaction of nursing staff and effects on patient safety. In an effort to examine how Texas nurses across the state are affected by the use of EHRs, the Texas Organization of Nurse Executives (TONE) and Texas Nurses Association (TNA) created a joint-Health Information Technology Committee to evaluate the usage and usability of electronic health records. The resulting committee formulated a research project aimed at establishing baseline measures of satisfaction. The statewide survey was implemented in 2014. Results have been analyzed with suggested improvement strategies to be deployed in 2016 and 20174. Outcomes of the survey are reported in Texas Nursing Magazine, Winter-2016 edition. The study engaged over 1,150 nurses across Texas.
Major findings include:
- 62.9% of nurses responding agreed or strongly agreed that overall, they prefer using the system over the old way of doing things, with 17.7 % of respondents indicating they disagreed or strongly disagreed.
- 60% indicated they believed they could depend on the system, with 40% disagreeing or strongly disagreeing.
- 57.8% indicated that they had adequate training, however, 12.9% disagreed or strongly disagreed that training was adequate.
- 54.4% reflected that they agreed or strongly agreed that the system had improved care, with 15.6% disagreeing or strongly disagreeing that care had been improved at their institution.
- 56.9% indicated that they believed errors are reduced with the system, with 12% disagreeing or strongly disagreeing that the system reduced errors.
- 55.7% noted that they strongly agreed or agreed that the system is more efficient than the old way of doing things, whereas 15.3% disagreed or strongly disagreed that the system is more efficient.
- 49.8% agreed or strongly agreed that the system improves practice and 16.2% indicated they disagreed or strongly disagreed that he system improves practice. 4 pp 7-8
Next steps include dissemination of information to nurse leaders across Texas, solicitation of input for improvement strategies, deployment of strategies and a follow-up study to determine the impact of interventions.
Members of the HIT Research Team are in the process of scheduling on site meetings with TONE and TNA Districts. The study will be presented directly to TONE members in the 2nd Quarter TONE Webinar.
More to come from this team, as investigation continues and implementation strategies are identified and implemented. As nurse leaders across the State, your feedback - innovations and recommendations related to the electronic health record - is vital in identifying needed change to increase satisfaction of nurses and improve the safety of all patients.