SOCIAL DETERMINANTS
COVID-19 Places a Spotlight on the Societal Factors that Influence Health
The COVID-19 pandemic has illuminated the social and economic circumstances that make some people more likely than others to become ill or have poor health.
The data are alarming: Latinos are nearly three times more likely to contract the virus, while Black individuals are more than twice as likely to die from it, according to the CDC. Underlying inequities are helping drive these numbers; for instance, 30% of white Americans are able to work from home during the pandemic, compared to 16% in the Hispanic community, the National Urban League reported. Higher rates of chronic conditions in these populations are only exacerbating the problems.
It has grown ever more urgent for hospitals to take steps to address the societal factors that lead to health inequities. “The pandemic has really placed a spotlight on the strong link between societal factors and health,” said Julia Resnick, senior program manager of strategic initiatives for the American Hospital Association. “It has created a burning platform to act.”
Food Insecurity
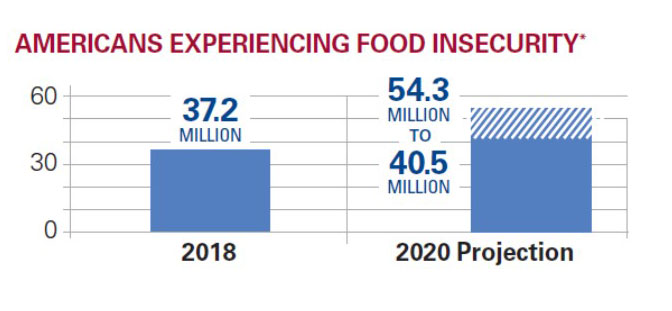 According to Feeding America, the number of Americans experiencing food insecurity is expected to grow to upward of 54 million in 2021 compared to 37.2 million in 2018. Again, minority communities are getting hit the hardest, with roughly one-third of Black and Latino Americans saying they have skipped a meal or relied on charity during the crisis, compared to just 8% of white individuals, a Kaiser Family Foundation poll found.
According to Feeding America, the number of Americans experiencing food insecurity is expected to grow to upward of 54 million in 2021 compared to 37.2 million in 2018. Again, minority communities are getting hit the hardest, with roughly one-third of Black and Latino Americans saying they have skipped a meal or relied on charity during the crisis, compared to just 8% of white individuals, a Kaiser Family Foundation poll found.
Health care organizations are getting creative in addressing this problem. Henry Ford Health System in Detroit, for example, has partnered with community groups to deliver food, personal protective equipment and other items to Black families.
The work is fueled by a partnership with the United Way of Southeastern Michigan and a $266,000 grant from Saving Our Selves: A BET COVID-19 Relief Effort. Henry Ford is executing a multi-pronged approach to address disparities, exacerbated by the crisis, in the Black community. To help community members avoid exposure to the virus, At Your Door: Food & More (AYD) is providing contact-free deliveries of food and supplies, alongside tailored educational materials, and tools to help individuals receive virtual support.
“Given the times, we believe AYD will provide a culturally relevant bridge to help restore trust in systems of care,” Kimberlydawn Wisdom, M.D., chief wellness and diversity officer at Henry Ford Health System, said in a statement.
Housing Insecurity Also a Challenge
Meanwhile, housing instability is also a growing concern for hospitals and health systems amid the pandemic as mounting job-loss numbers leave individuals unable to pay their rent or mortgage. About 16% of Americans said they’ve struggled covering housing costs, a number that climbs to 26% in among Latinos and 28% for African-Americans compared to 11% among whites, the Pew Research Center found.
 To address these concerns, the University of Arkansas for Medical Sciences has developed a screening tool to gauge patients’ ability to self-quarantine if testing positive for COVID and connect them a shelter. UAMS was able to develop its Ability to Self-Quarantine Screener and integrate it into the electronic health record in 30 days.
To address these concerns, the University of Arkansas for Medical Sciences has developed a screening tool to gauge patients’ ability to self-quarantine if testing positive for COVID and connect them a shelter. UAMS was able to develop its Ability to Self-Quarantine Screener and integrate it into the electronic health record in 30 days.
The tool has shown some early success, resulting in four avoided discharges to homeless shelters, and identifying 17 referrals to social workers for specific quarantine needs. Three more patients were designated for placement into state facilities designed for quarantining housing-insecure patients, according to an analysis published in the New England Journal of Medicine.
Sheppard Pratt — a Maryland-based private, nonprofit provider of mental health, substance use, special education, developmental disability and social services — has also increased its focus on addressing housing inequities amid the pandemic. Chief of Community Development Sarah Norman noted that in January an estimated $32 billion in back rent is coming due for Americans, likely triggering a wave of evictions, according to Stout Risius and Ross.
“You can’t talk about housing without talking about racism, and you can’t talk about fair housing without challenging the overwhelming stigma and disability discrimination still associated with mental illness,” Norman said.
To help address the problems, Sheppard Pratt utilizes service-enriched housing that is either owned or leased by the organization or one of its affiliates and is bolstered by evidence-based practices, including:
- Supported employment
- Assertive community treatment
- Motivational interviewing
All told, the initiative offers supportive housing for more than 1,000 residents.
“Unfortunately, discrimination has proven a significant barrier to affordable housing for people with disabilities,” Norman said.
Sheppard Pratt also offers rehousing services aimed at quickly getting clients off the streets. Those come coupled with financial assistance for rent and housing location services. In addition, intensive case management is available that links individuals with transportation, employment, childcare, behavioral health and legal assistance programs.
The organization served nearly 1,200 veterans and family members through its supportive services in fiscal year 2019, offering rent relief, security deposits, motel rooms and other resources. About 69% of participants are Black and 27% are white. The effort emphasizes “veterans helping veterans” with a peer-to-peer model that promotes long-term stability.
“Housing has always been a health intervention, but the pandemic has underscored just how essential a ‘home’ is to one’s health,” said Norman. “You can’t socially isolate if you’re sharing a couch with relatives or sleeping on the streets.”
Role of Planners and Marketers
Planners can play an important role in helping providers develop strategies to combat food and housing insecurities and other societal factors that influence wellness, the AHA’s Resnick added. “Hospitals and health systems are increasingly addressing the societal factors that influence health in their strategic plans, and planners can make a difference by being catalysts for furthering this important work in their organizations and the communities they serve,” she stressed.
Resnick said health care marketers are also vital in getting the word out to patients and the public about what their organizations are doing in this arena. “I would challenge marketers to connect with those in their hospitals and health systems who are leading initiatives focused on the societal factors that influence health. Learn about the efforts and find ways to promote them so that they can increase the impact of their work,” she said.
|
Resource from the AHA The American Hospital Association has developed a new resource — the Societal Factors that Influence Health: A Framework for Hospitals — to support hospitals in developing strategies to address the social needs of their patients, social determinants of health in their communities and the systemic causes that lead to health inequities during the COVID-19 pandemic and beyond. Additionally, the association’s Center for Health Innovation recently detailed the five actions hospitals can take to promote housing access during (and after) the crisis. |
This article features interviews with:
Julia Resnick
Senior Program Manager, Strategic Initiatives
American Hospital Association
Chicago
Sarah Norman
Chief of Community Development
Sheppard Pratt
Baltimore
Image credits: istock.com/Vladimir Vladimirov | Monkey Business Images/Shutterstock.com