MARKETING & DEI
The Role of Health Care Marketers in Equity Programs: Achieving Justice, Starting with Behavioral Health
Health care marketing teams can improve data collection, engage diverse communities, and remove communication barriers to improve behavioral health care for communities of color.
Events sparked by the murder of George Floyd compounded by stressors of the COVID-19 crisis are igniting new health equity campaigns and programs across American hospitals and health systems. These efforts seek to eliminate racial-ethnic disparities and identify, implement and embed culturally compassionate solutions to achieve favorable health outcomes.
Health care marketing, communication and strategy professionals play a critical role in hospital and health systems’ Diversity, Equity, Inclusion and Social Justice (DEIJ) strategic plans. To achieve goals of a DEIJ strategic plan, health care marketers must recognize the importance of moving beyond equity to achieve justice. While health care equality and equity translates to even access to care, achieving justice transcends equal opportunity by offering genuine care, treatment and respect to all patients.
“The concept that justice is the third part of the equality-equity-justice continuum is being incorporated into DEIJ strategic plans,” said Kimberlydawn Wisdom, MD, senior vice president of community health and equity and chief wellness and diversity officer at Detroit-based Henry Ford Health System in a recent AHA blog on Destination Justice. “It is increasingly evident to those of us who have traveled and fought on the equity road for over a decade that barriers must be removed for justice to ultimately be realized.”
From a medical perspective, constant exposure to stress is detrimental to one’s physical and mental health, and it is no surprise that pressures of the COVID-19 pandemic would exacerbate and present newer mental health challenges.
“As we have all dealt with the pandemic, there really isn’t any single person, family or community that hasn’t been impacted by COVID or the subsequent behavioral health consequences,” said Harsh K. Trivedi, MD, MBA, president and chief executive officer of Sheppard Pratt, the nation’s largest private, nonprofit provider of mental health, substance use, developmental disability, special education and social services.
“Post-COVID, we’re seeing opioid overdose rates at their highest since that epidemic began in the early ‘90s. We’re seeing how everyone is impacted by financial stress as well as stress of losing people in their lives or having medical consequences of COVID. … The behavioral health impact [post-COVID] will be massive because we know of the substantial relationship between overall health and behavioral health.”
Racial Disparities
The pandemic showed that communities of color were unevenly affected by the COVID-19 crisis. While the coronavirus took the lives of Black Americans at a disproportionate rate, low-income Black Americans also experienced greater job loss, more food and medicine insecurity, and higher indebtedness in the early months of the pandemic compared to other low-income communities. In addition, communities of color had substantially limited access to behavioral health care services.
Research also indicates Black Americans experience earlier health deterioration, as measured by biological indicators, when repeatedly exposed to and making adaption to chronic stress. In a race-conscious society, stigmatization and disadvantages built into the fabric of systems may cause disproportionate physiological deterioration.
“In order to dismantle these profound health disparities, we must address the structural and institutional aspects of racism that contributes to them,” said Dr. Wisdom. “As a result, individuals who have been systematically oppressed, disenfranchised and marginalized by current behavioral health systems face long-term side effects.”
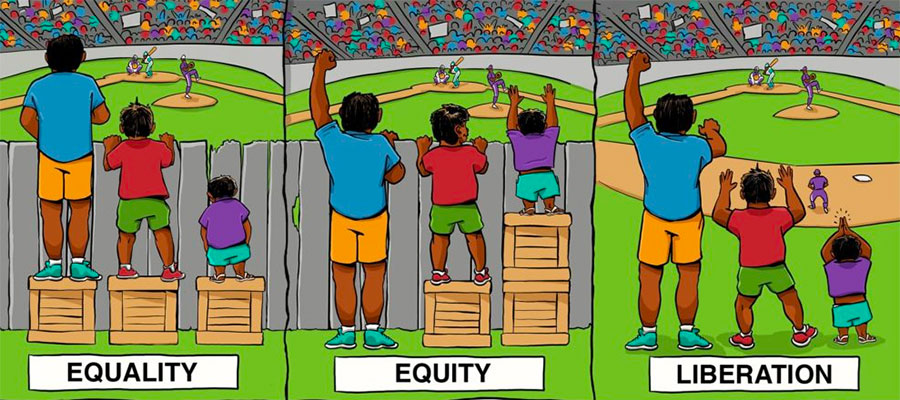
The Center For Story Based Strategy | Interaction Institute for Social Change | Artist: Angus Maguire.
How Health Care Marketers Can Help
Taking a proactive approach, health care marketing teams can improve data collection, engage diverse communities, and remove communication barriers to improve health outcomes and behavioral care gaps for their various patient populations. Health care marketers and communicators need to know who they are serving and whether disparities exist by collecting better self-reported data and stratifying that data by race and ethnicity.
“It’s important to get to know what your community needs and direct resources to address those issues,” said Dr. Trivedi.
Dr. Wisdom calls for a deeper dive on patient data to enhance care delivery. In 2011, she helped her employer Henry Ford Health System launch their “We Ask Because We Care” campaign to improve its collection of patient data, which earned them to be recognized as a 2021 Carolyn Boone Lewis Equity of Care Award Honoree by the American Hospital Association’s Institute for Diversity and Health Equity.
In 2020, several Henry Ford system hospitals exceeded a goal to collect race, ethnicity and language preference information from more than 90% of patients. The data has helped the health system better understand patient barriers, such as housing, transportation and food access, to improve care outcomes. More than 79,000 screenings were performed in 2020 to assess and develop a plan to address these societal factors.
In addition, the first clinic to offer rapid COVID-19 testing in the U.S. was launched in partnership between Henry Ford and the Detroit Health Department. Through this initiative, Henry Ford administered more than 20,000 tests to first responders and essential workers in Detroit. Henry Ford was the only Michigan health system to have a role in the Moderna vaccine trial, in which 30% of the enrolled participants were people of color. Throughout the pandemic, Henry Ford has prioritized reducing disparities in outcomes in diabetes, hypertension, and mortality and morbidity related to COVID-19.
In addition to improving data and making community partnerships, heath care marketing and communication professionals are in the unique position of helping to identify and remove barriers in behavioral health with messaging that is accurate, culturally competent, relevant and appropriate to specific communities of color and ethnicities being addressed.
“Behavioral health isn’t a vanilla diagnosis in the sense that it makes up a number of different conditions,” said Dr. Trivedi. “Different people need different interventions, to either feel comfortable or feel better … a one-size-fits-all solution isn’t going to work for every person, so that is where we need to get nuanced [so] each person can get the right help that they need. It needs to go beyond what we’ve done traditionally.”
According to the American Psychiatric Association, a lack of cultural understanding by health care providers may contribute to under-diagnosis and/or misdiagnosis of mental illness in people from racially or ethnically diverse populations. Factors that contribute to these kinds of misdiagnoses include language differences between patient and provider, stigma of mental illness among communities of color, and cultural presentation of symptoms. All of this can impact how someone perceives or describes their symptoms, the types of treatment they will accept, or if they seek treatment at all.
In the future, Dr. Wisdom hopes DEIJ strategic plan efforts become naturally ingrained in the processes and protocols of health care delivery so committees are no longer needed to close health care gaps. She envisions a routine surveillance mechanism that identifies gaps as early as possible, systematically and thoughtfully uses best practices to close those gaps, and continuously monitors to ensure gaps stay closed.
“In time, I hope the road to equity will be paved with interventions that make the highway barrier free and, with collective efforts from us all, we can accelerate the work towards that destination of justice,” said Dr. Wisdom.
Learning More
- This article features content from an AHA blog, “Destination Justice – Now Is the Time to Move Beyond Equity to Justice ... Starting With Behavioral Health”
This article features:
Harsh K. Trivedi, MD, MBA
President and Chief Executive Officer
Sheppard Pratt
Baltimore, Maryland
Kimberlydawn Wisdom, MD
Senior Vice President of Community Health and Equity and Chief Wellness and Diversity Officer
Henry Ford Health System
Detroit, Michigan


