The 2017 Hypertension Guideline Update and the Need for Revised Clinical Content
![]() Print this Article | Send to Colleague
Print this Article | Send to Colleague
Pat Stricker, RN, MEd
Senior Vice President
TCS Healthcare Technologies
Being a nurse, educator, and content developer for years, the news of the 2017 update to the Blood Pressure (BP) Guidelines made me immediately think about the number of revisions that will need to be made to written documents, audio/video media, and computerized programs that contain hypertension (HTN) information. Examples of these include patient education materials, standard patient letters that reflect HTN information, training materials, reports and reporting parameters, predictive analytic programs, related clinical guidelines, clinical content, care plans, treatment protocols, triage guidelines, algorithms, websites, BP and hypertension apps, etc. I know this type of change seems routine to most people, but when you are responsible for making these revisions it can be a large, time-consuming task. If you are not responsible, you still may want to get more information about the changes, so you can feel confident when explaining them to patients. So I thought I would focus this article on finding additional information that you can use to increase your own knowledge and to revise your HTN materials. However, let’s take a look at the changes that were made first.
On November 13, the American College of Cardiology (ACC) and the American Heart Association (AHA) announced the release of the "2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults". It was developed by the Task Force on Clinical Practice Guidelines that consisted of representatives from the ACC and AHA, along and nine other professional organizations[i]. This is the first time the hypertension guideline has been updated since "The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure" (JNC7) was released in 2003, 14 years ago.
The ACC/AHA Task Force consisted of 21 scientists and health professionals who reviewed over 900 studies and articles related to blood pressure monitoring, risks, treatment goals and strategies, thresholds to initiate anti-hypertension treatment and control, and various other topics. They found that the risks of heart disease, stroke, aneurysms, kidney disease, and vision disorders increase with systolic BPs over 120 mm Hg and that BPs of 130/80 mm Hg can double the risk. That was significant!
It did not mean that the risk factors had changed or increased; it meant that it is now apparent that blood pressures at a lower threshold can increase risks more than originally thought. This is a good thing. It means we can identify and treat individuals sooner, before serious complications occur as a result of the "Silent Killer" – Hypertension. It also means that the "pre-hypertension" classification of 120-139/80-89 mm Hg now needs to be changed to "elevated BP" and "hypertension" and treated as such. The majority of these individuals will be able to be treated with lifestyle changes (proper diet, exercise, weight loss, reduced smoking and sodium intake, and stress reduction) to reduce their BP to normal limits, thereby eliminating the need for medications and reducing their risks of more serious medical complications.
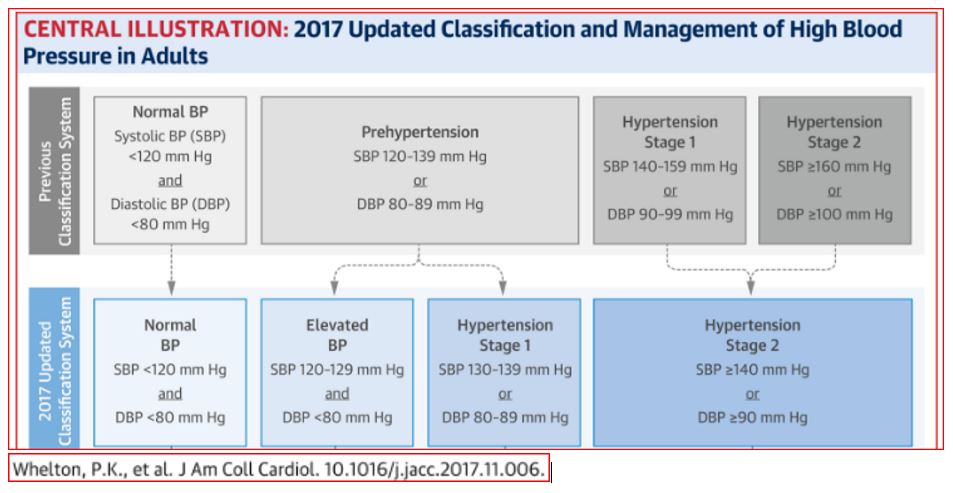
The following graph shows a comparison of the 2003 and 2017 BP classifications. The 2017 guideline:
- Eliminates the "Pre-hypertension" category and replaces it with:
- "Elevated BP" which is 120-129 and <80 mm Hg, and
- "Hypertension Stage 1" that is now identified as 130-139 or 80-89 mm Hg
- Lowers the BP in "Hypertension Stage 2" category to >140 or >90 mm Hg.
- There is also a "Hypertensive Crisis" category for patients with BP >180 and/or 120 mm Hg.
Once the guideline and treatment criteria were determined, the Task Force needed to determine what significance these BP changes would make to the prevalence of HTN in the U.S. They analyzed data from a 2011-2014 survey of over 9,000 records of adults who had their BP measured three times following a standard protocol. The average BP was weighted and compared with BP data obtained using the 2003 JNC7 guidelines in order to make predictions about how the 2017 changes would impact the U.S. population. Using the 2017 guidelines:
- 31 million more people will be diagnosed with HTN, increasing the overall prevalence of HTN in the U.S. to 103.3 million people.
- The prevalence of HTN among U.S. adults (> age 20) will increase from 31.9% to 45.6%, an increase of 13.7%.
- The number of adults (> age 45) with HTN will triple for men and double for women.
- 9.4% of U.S. adults may be treated with non-pharmacological interventions (lifestyle changes) instead of medications.
- The use of anti-hypertensive medications will increase from 34.3% to 36.2%.
- 81.9 million adults will be treated with medications.
While these statistics look overwhelming, they actually will provide more individuals with the ability to identify their risk much sooner, thereby allowing them to make lifestyle changes to reduce their risks and hopefully eliminate the need to take medications or progress to more serious medical complications as a result of HTN.
One of the ACC documents outlines 21 points to remember about the Guideline and the last one seems to sum up the intent of the guideline and goals for using it.
"Every adult with hypertension should have a clear, detailed, and current evidence-based plan of care that ensures the achievement of treatment and self-management goals; effective management of comorbid conditions; timely follow-up with the healthcare team; and adheres to CVD evidence-based guidelines. Effective behavioral and motivational strategies are recommended to promote lifestyle modification. A structured team-based approach including a physician, nurse, and pharmacist collaborative model is recommended, along with integrating home-based monitoring and telehealth interventions. Outcomes may be improved with quality improvement strategies at the health system, provider, and patient level. Financial incentives paid to providers can be useful."
Now that you are aware of what the changes are, let’s take a look at what the ACC and AHA have made available for everyone on their websites. Remember all those items I said that organizations were going to have to revise? Well, the ACC and AHA have already updated their websites to reflect the 2017 guideline changes. So you can use their information to increase your knowledge and make revisions to your content. There is a wealth of knowledge on each site, so I have listed some of the material that seems to provide the most useful information. There is also a lot of additional detailed treatment information for each BP classification that is not listed below. Each website has similar documents, so I have made notes (in bold italics) next to the documents that seemed to be more concise or easier to use.
The American Heart Association website provides easy-to-read content for healthcare professionals and patients.
- New Hypertension Guideline Updates How We Measure and Treat High Blood Pressure – News Release
- 2017 Hypertension Clinical Guidelines – Overview and Links to numerous documents
- Systematic Review – Description of research
- National Health and Nutrition Examination Survey (NHANES Survey) – Overview of Survey used for research data
- NHANES Data Source – Data source for 4 year research study to determine changes needed to guidelines and for comparative data to make predictions of how changes would impact the U.S. population; Good document for those wanting to review the data
- Highlights of 2017 Guideline – 2 page summary of the 2017 Guideline
- Hypertension Highlights 2017- Good detailed summary of Guideline with charts and graphs
- Top Ten Things to Know about the 2017 Hypertension Clinical Guideline – Good summary of key points.
- Slide Presentation – PDF version of the slides; Actual PPT slides available on ACC website
- Nearly half of U.S. adults could now be classified with high blood pressure, under new definitions - News article
- Don’t just get your BP taken; make sure it’s taken the right way - News article
- More than half of all African-Americans have high blood pressure under new diagnostic guidelines - News article
- High blood pressure redefined for first time in 14 years: 130 is the new high – News article
- Prevalence of US Adults with Hypertension – Graph
- Prevalence of US Adults Recommended for Pharmacological Treatment – Graph
- Tools & Downloads - For Diagnosis, Treatment Plans, Monitoring, Patient-Measured BP, and Best Practices
- AHA Guideline Apps – The website does not show the new HTN Guideline in the picture, but once you load the app it will ask if you want to update new content. It then adds the HTN guideline content.
- ACC/AHA ASCVD Risk Calculator
- ASCVD Risk Calculator
The American College of Cardiology website provides more clinically focused content.
- New ACC/AHA High Blood Pressure Guidelines Lower Definition of Hypertension – News release
- 2017 Guideline For the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults – Comparison graph of 2003 and 2017 guidelines and links to the full Guideline
- 2017 Guideline – full 193 page Guideline
- 2017 Guideline for High Blood Pressure in Adults: 21 Key Points to Remember
- 2017 Guideline_Made_Simple – Good collection of tables and graphs
- Guideline Hub | High Blood Pressure – Resource page with links to Quick Reference documents:
- Systematic Review – Description of research
- Data Supplement – Summaries of research articles used
- 2017 Guideline for High Blood Pressure in Adults – Key Points to Remember
- Guideline Analysis: Potential U.S. Population Impact of the 2017 High Blood Pressure Guideline – Summary of how predictions were determined
- 2017 Guideline Slides – Actual PowerPoint Slides
- Patient Education
- New Guidelines for High Blood Pressure – Good selection of CardioSmart Patient Education and Fact Sheets
- High Blood Pressure – Sample of Patient Education Sheet – BP overview, Lifestyle changes and Medications
- Guideline Clinical Apps - For Apple IOS on iTunes; the Android version does not appear to have the HTN guideline
I hope these will help you be able to navigate the websites a little easier and find the key information you need more quickly and easily.
REQUEST: I want this column to meet your needs. So if you have suggestions for specific types of information you would like presented or topics you would like researched, please let me know. You can contact me at pstricker@tcshealthcare.com.
[i] Other Associations represented on the Clinical Practice Guidelines Task Force: American Academy of Physician Assistants (AAPA), Association of Black Cardiologists (ABC), American College of Preventive Cardiology (ACPM), American Geriatric Society (AGS), American Pharmacists Association (APhA), American Society of Hypertension (ASH), American Society of Preventive Cardiology (ASPC), National Medical Association (NMA), and Preventive Cardiovascular Nurses Association (PCNA).
Pat Stricker, RN, MEd, is senior vice president of Clinical Services at TCS Healthcare Technologies. She can be reached at pstricker@tcshealthcare.com.
