|
|||||||||||||||||||||||||||||
| February 6, 2025 | |||||||||||||||||||||||||||||
Source: CT News Junkie, Feb. 5, 2025
Gov. Ned Lamont released a two-year, $55.2 billion budget proposal for the upcoming 2026-2027 biennium on Wednesday with a focus on expanding access to child care, providing a small tax cut to Connecticut residents, and allowing for some small but significant changes to the state’s hotly debated fiscal guardrails.
Lamont’s budget would spend about $27 billion in the upcoming year – a 3.8% increase from current funding levels. That amount would jump another 4.6% in 2027 to $28.2 billion.
Source: The CT Mirror, January 28, 2025
The Connecticut Mirror reported on January 28, 2025, that Connecticut Senator Matt Lesser (D-Middletown) and Representative Jillian Gilchrest (D-West Hartford) have introduced a plan to broadly increase Medicaid provider rates. The $250 million three-year plan aims to increase rates to be at least 75 to 80 percent of current Medicare rates, beginning with a $75 million funding infusion in 2026. The proposal would also establish a process to review and update provider rates every two to three years. The rate increase would not affect major hospital systems, which are subject to a settlement agreement expiring in 2026, but would affect the rates at specialty hospitals and Connecticut Children’s Medical Center.
Calling all Medicaid providers…WE NEED TESTIFIERS for this year’s public hearing to address the Human Services Medicaid portion of the governor’s budget, which will be held on Monday, February 24th beginning at 4 p.m. Both in-person and virtual options are available. Notify Tracy Wodatch if planning to testify (wodatch@cthealthcareathome.org).
Let your voice be heard. Tell your agency story about the impact of 17 years of no funding to the budget for Medicaid providers. The Association will assist and support you through the process, along with providing you with a messaging template and full instructions. Since September, the Healthcare Workforce Safety Working Group, co-chaired by Tracy Wodatch and Sasa Harriott, has been meeting to review and make recommendations on the recent safety laws passed in 2024 through Public Act 24-19 , Sections 1-4, 6. On Friday, January 31st, the working group submitted its final report.
Highlights of the recommendations include further transparency on information shared through the referral process, clarification of training, request for further funding and potential for ongoing working group efforts into 2025. The Association will continue to work toward supporting its members through compliance with the laws and, most importantly, a focus on evidence-based best practices.
Source: McKnights Long-Term Care News, January 30, 2025
A program that provides palliative care to people with dementia and their caregivers lowered the number of emergency department visits and hospitalizations by approximately half in about a year, a new study shows. Those who benefitted the most from the Indiana Palliative Excellence in Alzheimer Care Efforts (IN-PEACE) initiative were Black people and those with lower incomes. A report detailing the findings was published in JAMA ... The 50% decrease in emergency department visits and hospitalizations among people who received the intervention shows that the program can keep some people with dementia out of the hospital, where they can develop complications and functional declines. Source: Alliance Daily, February 3, 2025
The Alliance submitted comments on the proposed Contract Year 2026 Policy and Technical Changes to the Medicare Advantage (MA)Programs.
The proposed rule addresses refinements for several existing provisions aimed at protecting MA plan enrollees. While the rule does not address home health specifically, certain proposals have implications for Medicare beneficiaries that may be of interest to providers delivering care in the home. Source: McKnights Home Care, January 31, 2025
Medicare Advantage beneficiaries use significantly less end-of-life home health services compared with traditional Medicare enrollees, according to a new study published in JAMA Network Open.
The study found that traditional Medicare beneficiaries had a 4.2% higher rate of home health use at the end of life compared to MA beneficiaries. Approximately 37.5% of decedents enrolled in MA used end-of-life home healthcare, compared with 41.7% of traditional Medicare beneficiaries.
Source: McKnights Home Care, January 31, 2025
President Donald Trump’s immigration policies pose significant risks for home care providers, making it crucial for agencies to understand how to best protect their staff and operations in the event of U.S. Immigration and Customs Enforcement (ICE) investigations.
“The home care industry is already experiencing a shortage of qualified workers and individuals entering the workforce,” Angelo Spinola, a shareholder with Polsinelli, told McKnight’s Home Care Daily Pulse Friday in a statement. “Anti-immigration policies and deportations may aggravate that issue.”
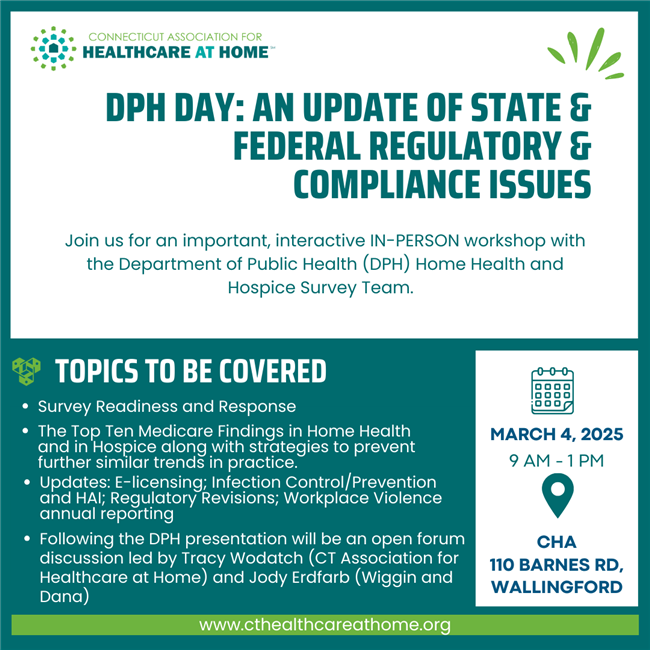
Join us for an important, interactive IN-PERSON workshop with the Department of Public Health (DPH) Home Health and Hospice Survey Team.
How they got started...
The idea for CareXM began in a single moment, several years ago, during one patient’s chemotherapy treatment at home. As his nurse prepared meticulously to change his sterile port, her mobile work phone interrupted with a buzz. In an instant, the look on her face changed from focused patient care to worry. The patient suddenly felt vulnerable as he read the dilemma on her expression: Should she continue with his procedure or take the incoming call from another patient in need?
In that moment, the chemotherapy patient wondered if there was a way to use his background in call routing technology to help this nurse—and countless others like her—to solve her dilemma. What if this nurse could use a mobile app to tell her team to forward patient calls to other available nurses so she could focus completely on her patient’s procedure? It would completely transform the care experience for both the nurse and the patient. The nurse ended up taking the new patient’s call and then carefully restarted his procedure with the same wonderful care she’d always given him. The patient’s worry ebbed as the new idea began to take root in his mind. Following his successful treatments, he began working on his idea with a team of hospice nurses who experienced the same kinds of interruptions as his own nurse. With their clinical expertise and the rest of his team’s call technology background, they created what is now CareXM.
|
|||||||||||||||||||||||||||||
| Past Issues | Subscribe | cthealthcareathome.org | Advertise with Us | |||||||||||||||||||||||||||||