
| Archives/Subscribe | Advertise | cmsa.org | cmsatoday.org | March 2014 |
What Is an "Average" Caseload? Pat Stricker, RN, MEd, Senior Vice President
TCS Healthcare Technologies How many times have we all heard (or asked) "What is the ‘average’ caseload?" Sounds like a simple question, doesn't it However, case management programs have struggled for years trying to determine realistic, standard caseloads. People are looking for "a number" that defines the average caseload, but in reality, there is no "magic" number.
Determining standard case loads is a challenge due to a complexity of factors across diverse CM settings. In addition, rapid changes in the medical management field have added to those complexities, e.g. the integration of utilization management (UM) and disease management (DM) into case management (CM) functions, and the increase in complex, condition management strategies. Some care management applications promote standardized workflows and acuity levels that can help determine caseloads and acuity levels for a given population. However these applications usually lack evidence-based algorithms to determine distinct, accurate, and realistic caseloads.
Literature reviews and other research findings on this topic cite caseloads that are focused on specific clinical or program areas, which make it difficult to generalize. In fall 2008, the Case Management Society of America (CMSA) and the National Association of Social Workers (NASW) published the Caseload Concept Paper to try to fill-in long standing gaps in this area. Their research found "average caseloads" ranging from two to 365!
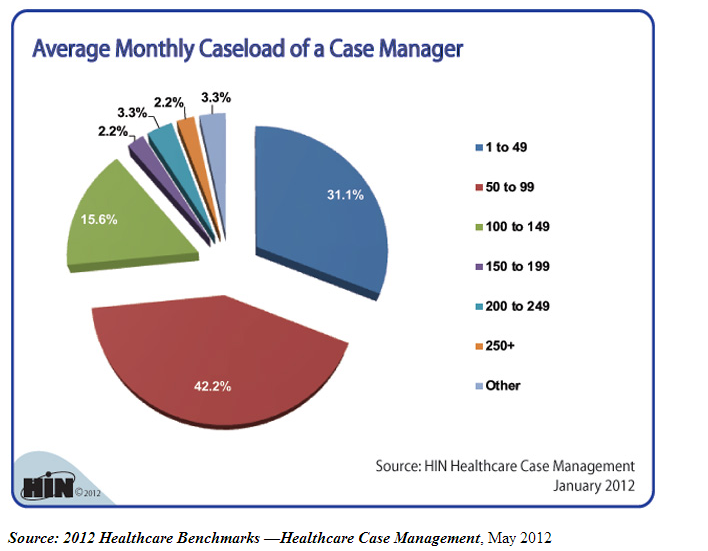 This graph from the Health Intelligence Network shows the average monthly caseloads reported in the 2012 Healthcare Benchmarks: Healthcare Case Management. This graph from the Health Intelligence Network shows the average monthly caseloads reported in the 2012 Healthcare Benchmarks: Healthcare Case Management.More recently an online nursing chat site identified caseloads ranging from 28 to 350!
How can these ranges be so different? The disparity is due to a variety of factors that affect the "average" caseload. The CMSA/NASW Concept Paper provides a Caseload Matrix that defines the variables that tend to impact caseloads:
The addition of integrated care management interventions, complex condition management programs, and provider-based accountable care organizations have also added to the dynamic nature of determining what the "right" caseload is in any given situation.
As a result of the above study, CMSA developed a free Case Load Capacity Calculator that provides rules and weights based on industry research and expertise. It can be used to calculate comparative caseload capacities across teams of case managers specific to the domain and setting in which they practice. It gathers information about the variables noted above and allows organizations to customize the tool to accommodate for differences in care delivery. CMSA has given us a great start by providing the concept paper and calculator, but we all need to work together to help define average caseloads for various types of programs. I encourage all of you to try the tool. Inputting your data will help you see how the various factors affect your caseload, as well as help contribute to the overall empirical data that is needed to determine the appropriate "average" caseload. CMSA also continues to sponsor other initiatives to determine the "average" caseload. For the past six years, CMSA has co-sponsored the Health Information Technology (HIT) survey with TCS Healthcare Technologies (TCS), and the American Board of Quality Assurance and Utilization Review Physicians, Inc. (ABQAURP). A core objective of the bi-annual survey was to identify how HIT applications impact the case management industry. Schooner Strategies (dba Schooner Healthcare Services), which conducted the surveys, has published a series of Trend Reports analyzing the results. Trend Report #7: Caseloads, focuses on care manager caseloads and time allocation. The survey asked respondents to estimate how many cases they handle per week, and describe how their time is allocated between various tasks, such as direct and indirect patient communication and administrative tasks. The report includes several figures and tables that analyze:
The survey questions looked at weekly caseloads, as opposed to the total number of cases that might be assigned to a care manager, to generalize the data across various settings. 26.5% of the respondents said they had 25-49 cases, 19.5% had 10-24 cases, 15% had 50-74 cases per week and 11.5% reported having over 100 cases per week. 16% indicated they did not have a routine caseload (i.e., management and administrative staff).
Case managers working in provider settings (behavioral health facilities, home care, hospital or health systems, medical group/clinic settings, retail clinics, skilled nursing or long-term care facilities) consistently reported having an average caseload of 25-49 cases. In addition, 62% of the case managers working in a home care setting reported having less than 50 cases per week, with 22% of that group supporting one to nine cases per week. Case managers in research centers or academic medical settings (29% of the respondents) were the outliers. They only reported having one to nine cases each week. The survey also asked respondents to indicate how much time they spend with patients and how much was devoted to performing other duties on a weekly basis:
Caseload levels were also compared with activities to determine the relationships with average time allocations. The highest face-to-face contacts were found in programs where case managers have between 120 and 174 weekly cases. These are usually in provider settings with short-term cases that require more immediate and defined tasks, such as in hospital or clinic settings, rather than in long-term, complex, telephonic case management programs.
The survey analysis supports the premise that variations in the delivery and settings for care management have a direct impact on the size of caseloads. A full copy of Trend Report #7: Caseloads and all other Trend Reports can be found here.
Will we ever be able to determine the average caseload? It seems unlikely that we will be able to define a specific number for an average caseload, but that doesn’t mean we should stop trying. We should continue to define caseloads for our specific programs, based on all the variables. More importantly, we need to share that data with one another so we come closer to finding that "illusive number."
To contact Pat Stricker, email her at pstricker@tcshealthcare.com, or reach her at (530) 886-1700 ext. 215. |
| The leading membership association providing professional collaboration across the health care continuum. 6301 Ranch Drive | Little Rock, AR 72223 | Phone: (501) 225-2229 | Toll-Free: (800) 216-2672 | Fax:(501) 221-9608 Secure Fax Line for Credit Cards: (501) 421-2135 | Email: cmsa@cmsa.org | Website: www.cmsa.org |